A coalition of community groups push to end AIDS at the epicenter of the U.S. epidemic
Beginning in January 2013, a coalition of New York HIV/AIDS leaders came together to begin a series of discussions to reenvision the state’s HIV/AIDS response. The goal was to encourage the state government to develop a New York State plan to end AIDS, applying the latest science, and building on implementation of the Affordable Care Act (ACA).
This initiative, organized by TAG and Housing Works and hosted by Wafaa El-Sadr, MD, MPH, at Columbia University’s Mailman School of Public Health, draws on the most recent science indicating that widespread HIV treatment can reduce new infections, and on the imminent implementation of health care reform through the ACA and Medicaid expansion. In October 2013, New York State will launch its state insurance exchange, while the federal government will begin to enforce the individual health mandate in 2014.
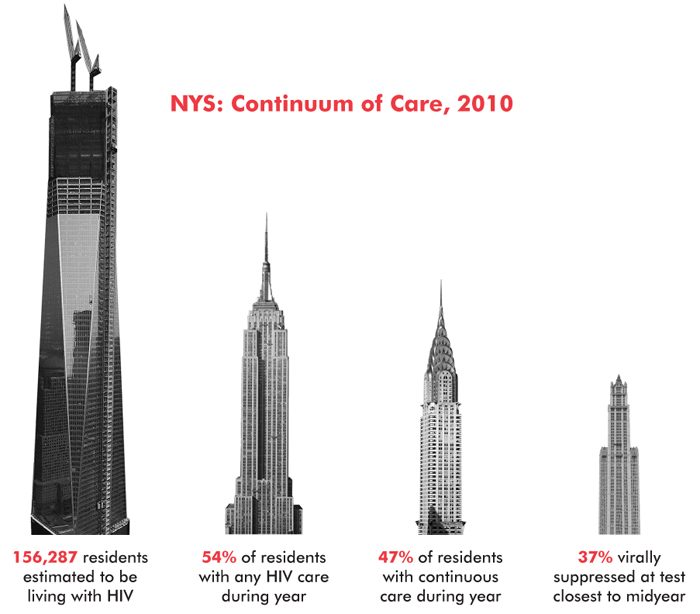
New York State remains the epicenter of the nation’s HIV epidemic. According to the state AIDS Institute, presenting at the second Housing Works and TAG meeting at Columbia in May 2013, new infections have dropped 36 percent since 2007. New infections in New York State dropped from 10 percent of the national level in 2007 to seven percent in 2010; yet it still has the largest number of people living with HIV/AIDS of any state. According to 2010 estimates, 156,000 people were living with HIV/AIDS in New York; at least 28,000 of them were unaware of their status; and only 37 percent had undetectable viral loads.
While the overall HIV incidence in the state has been decreasing, the rate of new HIV infections among men who have sex with men (MSM) and young MSM of color continues to rise disproportionately. Wide disparities along the continuum of care—including rates of diagnosis, linkage to care, retention in care, and undetectable viral-load rates—also continue to persist among underserved groups. Transgender people, women, youth, people of color, low income and homeless individuals, people who inject drugs, immigrants, and the formerly incarcerated are less likely to be engaged in care.
The rollout of the ACA in January 2014 is anticipated to cause massive shifts in the publicly funded health care delivery models for people with HIV in the state. For those who don’t have employment-based insurance, people previously barred from private insurance due to preexisting conditions can now access care through the NYS Health Benefits Exchange. While “navigators” are undergoing training to help people evaluate and choose a plan that meet all of their health care needs, with different levels of premiums, deductibles, and covered services, the process will be challenging. In Manhattan alone, there are nine individual plans and three small business plans. Individuals with incomes between 133 and 400 percent of the federal poverty level will receive subsidies and out-of-pocket support provided by the ACA.
People receiving care through Ryan White CARE Act–funded programs will likely be moved to either the expanded Medicaid, or transition to an Exchange plan with their premiums and deductibles covered by the AIDS Drug Assistance Program (ADAP), depending on their income. Ryan White programs will also be needed to provide support services such as case management, food, legal and linguistic services, housing, transportation, and psychosocial support programs required to keep people engaged in care and adherent to treatment.
Access, retention-in-care, and disparity issues were among the recurring themes raised during the TAG and Housing Works consultations in January and May of this year. Prominent New York City and State AIDS advocates, service providers, public health officials, and researchers came together to discuss where policy and funding gaps persist in our local and statewide HIV/AIDS response and how these gaps can be addressed using existing Ryan White program funding and new investments made in compliance with the state’s implementation of health care reform.
Overarching themes of the community consultations were improving the continuum of care in New York State by reallocating funding to better target those at greatest risk and refocusing on evidenced-based, high-priority interventions, especially treatment and prevention scale-up. Consultation participants discussed some of the innovative testing and linkage-to-care strategies already being used in some parts of New York City—the Bronx Knows campaign, for example, which surpassed targets initially set for the program—and explored innovative mechanisms for improving early antiretroviral therapy (ART) initiation; increasing the rates of ART utilization; addressing clinical care engagement challenges, notably persistent racial, ethnic, and age-related disparities; and maximizing common-sense HIV prevention services (e.g., greater access to free condoms and housing) for those at greatest risk.
Consultation panelists provided nuanced overviews of the challenges and successes of the San Francisco and Massachusetts community models, wherein reductions in HIV incidence were achieved over the past couple of years by scaling up a number of key evidence-based strategies for success, such as universal access to, and expanded utilization of, health care. Examples include health care provided in ways that are respectful of the needs of affected populations, investment in support for critical ancillary services (e.g., housing, nutrition, transportation, mental health, and supportive environments), and close and intensive communication among public health authorities, researchers, providers, and the HIV community.
Guaranteed universal access to lifesaving medications, treatment, and HIV prevention education will be essential for the health and quality of life of all New Yorkers. Advocates and service providers have long recognized the importance of regular, routine, accessible, and affordable care and services as a means of preventing transmission for those at risk of contracting HIV and for slowing the progression of HIV to AIDS.
In August 2013, Housing Works, TAG, and a coalition of community groups submitted a working paper to New York State’s deputy secretary of health, describing five key elements of a plan to end AIDS in the state; the working paper is now under review (an early draft can be accessed at here). It is hoped that during his 2014 State of the State address Governor Cuomo will fully recognize the need for a plan to end AIDS, and that he will announce the formation of a commission to implement this plan.
New York State, where, along with California, the epidemic first emerged in the United States, now has the chance to become one of the first states to commit to ending the pandemic. •
