Download:
October 2016
By: Suraj Madoori
Edited by: Erica Lessem, Kenyon Farrow, and Mike Frick
There is great hope for ending tuberculosis (TB)—the world’s leading infectious disease—thanks to both scientific progress and increased ambition from policymakers. But achieving this goal will require more investments in research and development (R&D). With funding trends distressingly on the decline for TB R&D, political action is critical to bend the curve up toward the development of breakthrough diagnostics, treatments, and vaccines needed to realize the promise of ending TB.
“Limited funding is impacting everything in our TB work. It impacts the speed at which new tools become available. The annual decline in research funding will be translated into failures in reaching any target in the Global Plan to End TB, World Health Organization End TB Strategy, and Sustainable Development Goals.” ~ Lucica Ditiu, Executive Director of the Stop TB Partnership
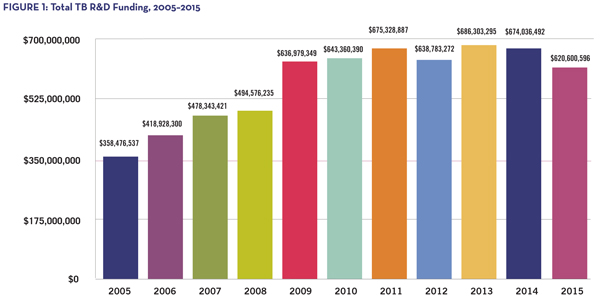
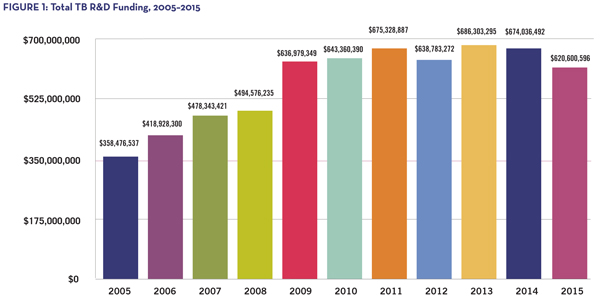
Investments for TB R&D fell by US$53.4 million in one year, plunging to a total of US$620.6 million in 2015.1 This represents the lowest level of funding for TB R&D since 2008 (see Figure 1) and is well below the US$2.2 billion annual target defined by the Stop TB Partnership’s 2011–2015 Global Plan to Stop TB.2 Funding for TB R&D has never totaled more than one-third of the projected amount needed to catalyze a scientific strategy to end TB, in line with the World Health Organization End TB Strategy.3
Despite inadequate funding, the global TB research community has had major successes, giving new hope to the response and demonstrating that investments in TB research foster great return for public health. Even with limited funding, researchers have developed several faster tests to diagnose TB—including drug-resistant strains and TB in people with HIV; new treatments to cure multidrug-resistant TB more effectively and faster; and shorter, easier preventive therapy that can stop latent TB from progressing to a deadly, infectious disease. But much more momentum is needed—tests are still complicated, treatment still takes months, and an effective vaccine is still elusive. Realizing the global vision of a world free of TB by 2035 (as set forth by the End TB Strategy) necessitates substantial commitment from governments to fund TB R&D.
 Political will is a cornerstone of the science-based response: government investments fund 63 percent of the total R&D for TB (see Figure 2). But 67 percent of total public funding comes from the U.S. government.4 The United Kingdom and the European Union are the next largest contributors to TB research. However, many high-income countries, as well as the governments of countries with a high TB burden, including the BRICS countries (Brazil, Russia, India, China, and South Africa), could contribute far more. Currently, the vast majority of TB R&D relies on a few key stakeholders, which places global funding in a precarious position, especially given the lack of private sector investment in TB due to its perception as an unprofitable market.
Political will is a cornerstone of the science-based response: government investments fund 63 percent of the total R&D for TB (see Figure 2). But 67 percent of total public funding comes from the U.S. government.4 The United Kingdom and the European Union are the next largest contributors to TB research. However, many high-income countries, as well as the governments of countries with a high TB burden, including the BRICS countries (Brazil, Russia, India, China, and South Africa), could contribute far more. Currently, the vast majority of TB R&D relies on a few key stakeholders, which places global funding in a precarious position, especially given the lack of private sector investment in TB due to its perception as an unprofitable market.
Expanding the base of public funding support for TB R&D is critical. It will stabilize research and ensure equitable sharing of the TB response and access to the benefits of science. Even a small boost in investments beyond nominal contributions from the BRICS countries would position them as leaders in the global rankings for TB R&D support. Increasing government commitments can also positively impact national economies and support growth of a biomedical research sector—a key component of many successful economies. To that end, political will remains necessary to scale up robust support for TB R&D from governments beyond the United States and achieve the tremendous scientific breakthroughs that are out of reach with current funding levels.
There is no time to lose: parliamentarians and leaders of representative governments have an important role in generating the political will necessary to enhance funding for global TB R&D. Policymakers must work across political divides in a nonpartisan, inclusive way and engage with civil society, researchers, and affected communities involved in the fight against the TB epidemic to prioritize these actions:
- Priority action #1: increase public funding for TB R&D. In 2015, civil society called on European countries to double investments in TB R&D and the BRICS countries to triple their contributions.5 These countries must heed the call to increase funding in 2016 and beyond. Australia and Gulf countries could also play a key role by investing more.
- Priority action #2: report publicly on TB R&D funding. More transparency on public TB R&D funding data is needed from countries that have not reported their investments—such as China, Russia, and the Gulf states. Countries should report data to provide a more complete global picture of R&D for TB and highlight their important contributions to the field. Countries seeking to take the next step can share TB R&D investment information by contacting Treatment Action Group at tbrdtracking@treatmentactiongroup.org.
“There can be no end to TB without an end to political indifference in this R&D agenda.”
~ Lynette Mabote, Team Leader, Regional HIV, TB and Human Rights Programmes, AIDS and Rights Alliance for Southern Africa
- Frick M. 2016 report on tuberculosis research funding trends, 2005–2015: no time to lose. Edited by Mark Harrington and Erica Lessem. New York: Treatment Action Group; 2016. Available from: www.treatmentactiongroup.org/tbrd2016. (Accessed 2016 October 1)
- Stop TB Partnership. The global plan to stop TB: 2011–2015. Geneva: World Health Organization; 2010. Available from: http://www.stoptb.org/assets/documents/global/plan/tb_globalplantostoptb2011-2015.pdf. (Accessed 2016 October 3)
- World Health Organization. The end TB strategy. Geneva: World Health Organization; 2014. Available from: http://www.who.int/tb/strategy/End_TB_Strategy.pdf?ua=1. (Accessed 2016 October 2)
- Frick M. 2016 report on tuberculosis research funding trends.
- Treatment Action Campaign et al. “We die of TB” TB is an emergency! [Internet]. 2015 December 3 (cited 2016 October 3). Available from: http://tac.org.za/sites/default/files/Memorandum_TB.pdf.
