What is screening?
Screening looks to see whether someone might have a disease. For hepatitis C virus (HCV), screening means looking for antibodies instead of the virus.
What are antibodies?
Antibodies are Y-shaped proteins made by a person’s immune system. They are part of the immune system’s response to viruses, bacteria, and other harmful substances (called antigens).
Antibodies attach themselves to antigens or infected cells and tag them so that other immune cells can find and disable them. Antibodies stay in a person’s body long after the antigen that triggered them disappears (this is called immunological memory). If the same antigen enters a person’s body again, even years later, the immune system will remember it—and send antibodies to destroy it.
When HCV enters a person’s bloodstream, it triggers an immune response. The immune system makes HCV-fighting antibodies. Sometimes, the immune system gets rid of hepatitis C virus by itself (this is called spontaneous viral clearance). About a quarter of people with hepatitis C will spontaneously clear the virus. This is more likely in young people (especially women), people who do not have HIV, and people with the IL28B CC genotype (refer to TAG’s Hepatitis C and the IL28B Gene fact sheet).
Even when a person has cleared HCV or been cured by treatment, HCV antibodies remain in a person’s blood for years.
What does a negative HCV antibody test result mean?
A negative antibody test result usually means that the person has not been infected with hepatitis C (unless they were infected very recently or have a weakened immune system).
The body needs at least two months (and sometimes up to nine months) to make antibodies. People with weakened immune systems (from an illness or certain medications) are not always able to produce antibodies. This might happen in people with autoimmune disorders (when a person’s immune system attacks his or her own organs or tissues), HIV-positive people with a CD4 cell count below <200 cells/mm3, and people taking immunosuppressants.
What does a positive HCV antibody test result mean?
A positive antibody test result means that a person has been infected with hepatitis C. It does not mean that the person still has hepatitis C. A different test, to look for the actual hepatitis C virus, is needed to make a diagnosis.
What is testing?
Testing will confirm—or rule out—whether someone has a disease.
How is a person tested for hepatitis C?
A viral-load test (called HCV RNA) is used to check for hepatitis C in the bloodstream. Usually, hepatitis C virus can be found in a person’s bloodstream two weeks after he or she becomes infected.
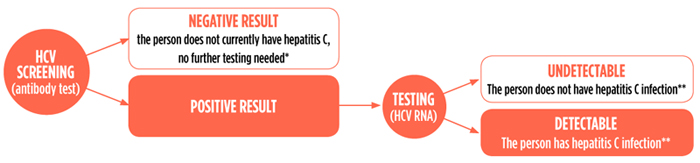
*Except in case of recent risk (within six months) or in people with a weakened immune system
**During the first six months after HCV infection, a person may spontaneously clear the virus; if there was a recent risk, repeat viral-load testing to confirm chronic hepatitis C infection
There are two types of viral-load tests: qualitative and quantitative.
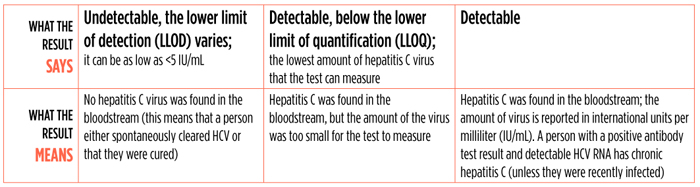
Qualitative testing checks whether there is hepatitis C virus in the bloodstream (detectable or undetectable).
Quantitative testing measures the amount of hepatitis C virus in the bloodstream. These tests are used during and after HCV treatment to see if it is working and whether a person is cured.
HCV Qualitative Testing
HCV Core Antigen Testing
The hepatitis C core antigen is a viral protein. Since the core antigen is part of hepatitis C virus, it can usually be found in the bloodstream two weeks after infection.
Since HCV core antigen testing is simpler and less expensive than viral-load testing, some experts suggest using it in resource-limited settings. Core antigen testing can be used—often with HCV antibody testing—to detect acute HCV or to confirm chronic HCV infection. HCV core antigen testing can also be used to measure treatment outcome. Although it does not detect low levels of HCV (<1,000 IU/mL), usually the hepatitis C viral load is much higher in people who relapse after HCV treatment.
HCV Genotyping
There are at least six known hepatitis C genotypes, numbered in the order that they were discovered. Each genotype has many subtypes, each given a letter in the order that they were discovered. People can be infected with more than one HCV genotype (called mixed infection). This is most likely to happen to people who got blood products or blood transfusions many years ago or in a place where the blood supply is not checked for HCV; people on kidney dialysis; or people who inject drugs with shared, unsterilized equipment.
Currently, the type and length of HCV treatment depend on which genotype a person has. Soon, it might be possible to use one HCV regimen for everyone (called pangenotypic), making HCV genotyping unnecessary.
Liver Disease Staging
The type and length of HCV treatment sometimes depend on how much liver damage a person has (for example, people with cirrhosis are often given ribavirin and treated longer than people who have less liver damage).
There are different methods to determine how much liver damage a person has (called staging). Although noninvasive tests are not always as precise as a liver biopsy, they are safer, less expensive, and easier to perform and undergo. It is becoming more common to use routine blood tests or ultrasound imaging to see whether a person has cirrhosis.
New HCV Diagnostics
Now that HCV treatment is simpler, safer, and more effective, diagnostics need to become simpler and less expensive.
Ideally, HCV will soon be diagnosed with a single rapid point-of-care test and cured with a pangenotypic regimen.

